In the ever-evolving field of healthcare, technological advancements have paved the way for groundbreaking procedures, one of which is robotic surgery. At Dhameliya Kidney Hospital, we pride ourselves on embracing innovation to offer our patients the highest standard of care. Robotic surgery is a minimally invasive technique that enhances precision, reduces recovery time, and improves overall surgical outcomes.
What is Robotic Surgery?
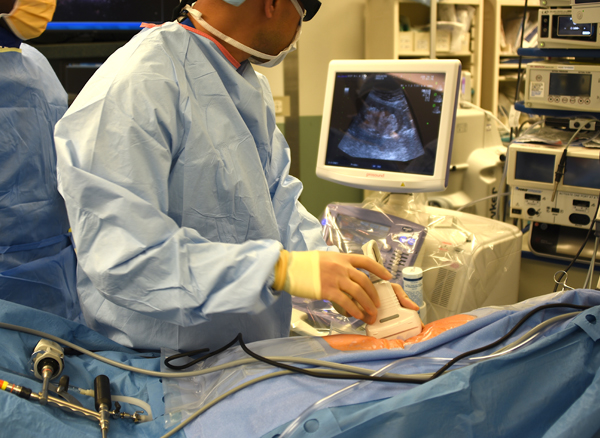
Robotic surgery utilizes advanced robotic systems to assist surgeons in performing complex procedures with unmatched accuracy. Operated by highly skilled surgeons, this state-of-the-art technology offers enhanced visualization, flexibility, and control, making it particularly effective for delicate surgeries involving the kidneys, prostate, and bladder.
How Robotic Surgery Works?
Robotic surgery employs a robotic platform equipped with:
Robotic Arms with Precision Instruments:-
The robotic arms can move in ways that human hands can't, such as rotating 360 degrees. This allows surgeons to perform delicate procedures in tight spaces.
High-definition 3D Visualization:-
High-definition 3D imaging gives surgeons a detailed view of the surgical site.The surgeon controls the robot, which allows for greater precision than the human hand alone.
Enhanced Dexterity:-
The surgeon operates the robotic system from a console, ensuring full control while leveraging the robot’s advanced capabilities for superior results.
The surgeon operates the robotic system from a console, ensuring full control while leveraging the robot’s advanced capabilities for superior results.
Benefits of Robotic Surgery:-
Robotic surgery offers significant advantages compared to traditional open and laparoscopic procedures:
- Minimally Invasive – Smaller incisions mean less scarring.
- Enhanced Precision – Greater accuracy for intricate surgeries.
- Faster Recovery – Shorter downtime for patients.
- Reduced Blood Loss – Minimizing complications.
- Less Pain – Enhanced patient comfort.
- Shorter Hospital Stay – Patients can return home sooner.
- Improved Surgical Outcomes – Higher success rates for complex procedures.
Applications of Robotic Surgery in Urology Care
At Dhameliya Kidney Hospital, robotic surgery is revolutionizing the way we treat complex Cancer conditions. Some of the common applications include:
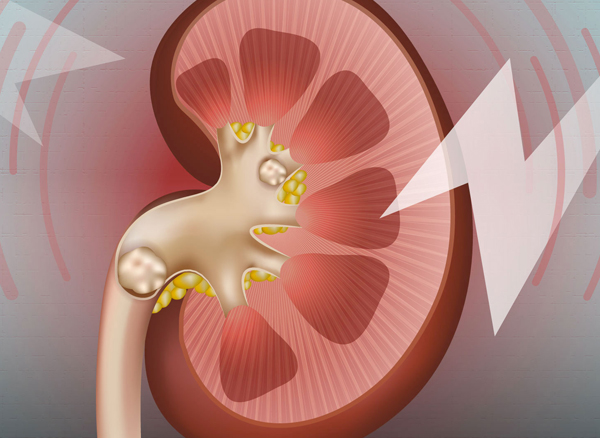
Kidney Cancer Treatment
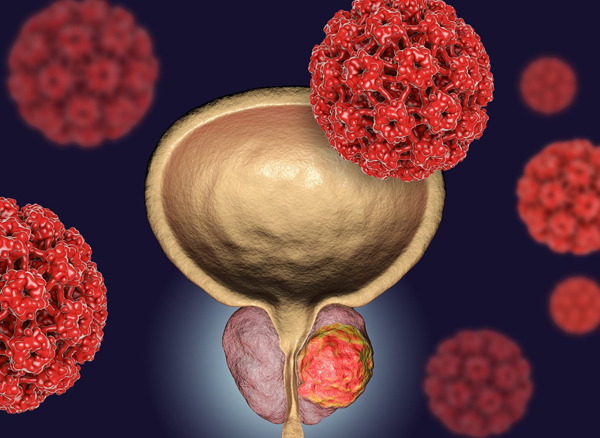
Prostate Cancer Treatment
Bladder Cancer Treatment
Reconstructive Surgeries
Why Choose Dhameliya Kidney Hospital?
Dhameliya Kidney Hospital is a pioneer in robotic surgery, offering patients cutting-edge solutions for urological care. Our approach combines advanced technology with compassionate care, ensuring the best possible outcomes.
Expertise You Can Trust – Our team includes highly skilled surgeons with extensive experience in robotic procedures.
Comprehensive Care – From diagnosis to recovery, we provide holistic support for our patients.
Patient-Centric Approach – Your health and well-being are always our top priority.
Learn More About Cancer Prevention and Care
Robotic surgery is just one aspect of our commitment to advanced kidney, prostate, and bladder care. With cutting-edge technology like 3D 4K vision, our robotic systems provide unparalleled precision, ensuring the most accurate and effective treatment for cancer.
Take the Next Step with Dhameliya Kidney Hospital
Whether you require robotic surgery or other specialized Cancer treatments, Dhameliya Kidney Hospital is your trusted partner in health. Contact us today to explore how robotic surgery can benefit you and schedule a consultation with our expert team.
By integrating cutting-edge technology with compassionate care, we are dedicated to improving lives and setting new benchmarks in kidney and prostate health.









389.jpeg)